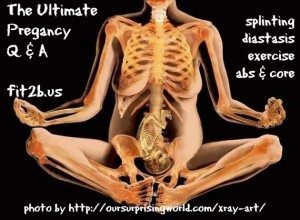
Pregnancy Q & A
The most common lament I hear is, “Why didn’t I know?”
You want to know why no one told you about diastasis recti, and you want to know why no one referred you to pelvic physical therapy for your prolapse and why no one offered you a splint when your pendulous belly interfered with your birth and recovery!
Perhaps you’ve begun to discover that these physical conditions are largely treatable and preventable, so you also want to know why your OBGYN said you’d need surgery to fix most of these issues (Hint: because they’re surgeons).
Why aren’t more women told how to prevent severe diastasis recti and pelvic floor issues prior to pregnancy, during pregnancy, and after they give birth? Why are these lessons seldom taught?
Below, you will find questions with my anecdotal answers, resources, and a few research study references to the most common questions I receive regarding pregnancy. First, though, I’d like to admit that I don’t know everything. Eight years into devoting my career to studying tummysafe fitness strategies, I know there’s still more to learn about diastasis recti and all its ramifications.
1. Can I avoid a Diastasis Rectus Abdominus (DRA) while pregnant?
No. Maybe. Sort of. It depends.
I get this question a lot (even with this page plastered everywhere), because dealing with diastasis recti is our niche specialty here on Fit2B.
But look, here’s the thing: your abs aren’t made out of rock. They are living muscles and innervated fascia, all responding in real time to various forces placed on them by load, nutrition, intra-abdominal pressure, stress, genetics, and many other things.
Your core is designed to stretch, flex, and bulge repeatedly throughout your life as it accommodates normal, healthy things like big meals, gas, pee, poop, laughter, coughing, growing babies, and giving birth.
Yes, for a long time, pregnancy was thought to be the only cause of DRA, but with men and children also experiencing it, we have to acknowledge that pregnancy isn’t the sole cause of ab gaps. Having devoted all my studies to this topic since 2008, my conclusions about the causes of diastasis recti are based on a pressure-tension model.
So—can you avoid DRA completely while pregnant? It’s not likely. Can you do some things to support your core and prevent that gap from widening to the point of a difficult recovery? Yes, and that brings us to the next question.
Helpful Resources:
- If you don’t know what DR is, download my free printable handouts.
- Read this article by biomechanist Katy Bowman: “Under Pressure.”
- Peek at this abstract of a study published in the 2015 Manual Therapy by Mota et al, which says, “The prevalence of DRA decreased from 100% at gestational week [down to] 35-39% at 6 months postpartum.”
- In a 1988 study by Blaschak and Boissonnault, “Diastasis recti abdominis was observed initially in the women in the second trimester group. Its incidence peaked in the third trimester group; remained high in the women in the immediate postpartum group; and declined, but did not disappear, in the later postpartum group.”
2. Can I heal my DR while pregnant?
A growing baby can create lots of pressure in your belly, but I’ve met and worked with many women who have managed to minimize their diastasis rectii and even narrow it a bit while pregnant.
Kelly Dean, a licensed physical therapist and owner of The Tummy Team, presented a couple of case studies at her workshop “The Importance of Core Strength in the Prenatal & Postnatal Client” regarding women who finished prior pregnancies with 4- to 6-finger gaps, closed them with physical therapy on their core, then went on to finish subsequent pregnancies with 2-finger gaps that closed within 6 weeks.
 Also, in the Fit2B forum, I’ve had quite a few clients report their abdominal gaps narrowing and even closing during the 1st or 2nd trimester. It goes like this: they find out they have diastasis at the same time they learn they’re pregnant. They start the work of aligning and targeting their transverse, and it closes a bit or evan all the way. Then baby grows, and belly expands, and maybe it opens up a bit toward the end of their pregnancy or during delivery.
Also, in the Fit2B forum, I’ve had quite a few clients report their abdominal gaps narrowing and even closing during the 1st or 2nd trimester. It goes like this: they find out they have diastasis at the same time they learn they’re pregnant. They start the work of aligning and targeting their transverse, and it closes a bit or evan all the way. Then baby grows, and belly expands, and maybe it opens up a bit toward the end of their pregnancy or during delivery.
I believe mismanaged abdominal pressure contributes to “wider than normal” abdominal separations when the deep core muscles are unable to generate the proper amount of tension to resist that pressure. I also believe that the way we move, eat, breathe, and align our bodies can alter the pressure put on our bellies. Thus, I teach my clients many body-positive methods to manage that pressure in order to minimize diastasis recti.
“Remember how I said I was starting to feel separation above and below my navel? Well after being very faithful with my alignment, tummy safe workouts and not letting my “guts spill on the floor” every time I bend over, I am happy to report that I no longer feel any separation! Which is amazing because my baby belly has grown quite a bit in the meantime!”
–Bethann W., 28 weeks pregnant
Resources:
- Look into the online prenatal physical therapy course offered by The Tummy Team.
- Watch this free video we did with a midwife who gets it!
3. Should I splint during or after pregnancy?
When the fascia of your abs is so strained that it can no longer maintain appropriate pressure, assist proper fetal alignment, or transmit force, I believe it needs some temporary support in conjunction with helpful exercises. Ideally, every woman should work with a women’s health physical therapist during and after pregnancy who will help minimize the need for splinting with personalized techniques.

Kelly Dean, LPT and founder of The Tummy Team, recommends splinting when a diastasis recti is 3 finger-widths or wider, and she also makes a strong case that splinting can help fight postpartum depression, regardless of the presence of diastasis recti. It is usually not necessary to splint during the first trimester of pregnancy, but it is often recommended for later stages if a DRA opens past 3 cm/3 finger-widths.
What about splinting after a C-section?
Always ask your care provider about this. I’ve asked around and discovered that it’s common practice in many hospitals in my area to provide splints after a multiples birth or Cesarean section but not for vaginal birth. Meanwhile, some hospitals don’t offer any splinting. There’s no consistency in America, but postnatal belly binding seems standard in other countries.
“The incision needs to be open to the air in order to heal,” said a labor and delivery nurse I spoke to in Connecticut. “We agree that binding is really, really beneficial but it’s secondary to caring for a wound, which takes priority—so always ask your surgeon.”
So perhaps this is one more reason to avoid c-section if possible: You may be advised to wait longer to support and connect with your core + there is often nerve damage from the cutting and pulling.
Overall, I believe every woman should be assessed for pelvic floor injury or severe dysfunction before she’s released by her hospital or midwfe. She should be provided with a referral to a quality core rehab specialist and offered a splint (not a corset, waist trainer, compression garment, or brace) with instructions for proper use. That’s a big dream.
Resources:
- Another article I wrote about “Binding Your Belly After Birth.”
- Click here to see my favorite 4 abdominal splints.
4. What moves should I avoid while pregnant?
When I was pregnant, I did all the things because I could do them. I felt fine. I felt powerful. I loved the comments I got on my strength. I reveled in setting an example for other pregnant women, showing them that pregnancy is a healthy, normal part of life that doesn’t need to slow us down.
I didn’t know much about diastasis back then. I braced my abs with my hands while I did crunches. I used dumbbells to row while I did planks. I had a healthy, strong birth + a healthy baby who weighed in bigger than those of my friends who didn’t exercise. Then I fell apart. My abs were distended, and I began leaking. After my second birth, I added sexual discomfort to my list of symptoms. I was told it was normal, to have a glass of wine, to use my estrogen cream more.
Just because you can, doesn’t mean you should.
I could have stayed in excellent shape and avoided things that I now know made my diastasis recti and pelvic floor take longer to recover.
So the quick answer to this question is that I think you should avoid crunches, sit ups, and unmodified planks during pregnancy and immediately postpartum until you have done core rehab, and then I think you should use my workouts to make a safe return to fitness.
A slightly more detailed, yet still generalized answer is that while you’re pregnant you should avoid any move that:
- makes your abs or crotch bulge . . .
- has you holding your breath . . .
- unbalances you to the point of falling . . .
- smashes your belly or leaves it hanging like a sack of potatoes toward the floor . . .
- causes bleeding, dizziness, nausea, or pain . . .
- doesn’t leave you feeling like a queen!
I have more than enough approaches to keep you moving in ways that will bless your body while you’re growing another body. That’s the beauty and fun of being a core fitness specialist, and I sure love teaching mamas new methods that truly help their tummies.
Resources:
- Read my “Top 5 Non-Crunchy Ab Moves” article & watch the free video with alternatives to doing crunches.
- Check out Kelly’s compelling argument against crunches in “Why Crunches Can Do Damage.”
- You may also want to be wary of over-squeezing your Kegels during pregnancy. Check out the “No More Kegels During Pregnancy” article from Positively Pregnant.
5. What motions should I focus on while pregnant?
 This is my favorite question, but I cannot spell it out in five paragraphs. Maybe I could—but I’d rather show you, so I made a lot of workout videos. Several of my Fit2B home fitness workouts are especially WONDERFANTABULOUSO when you’re preggers.
This is my favorite question, but I cannot spell it out in five paragraphs. Maybe I could—but I’d rather show you, so I made a lot of workout videos. Several of my Fit2B home fitness workouts are especially WONDERFANTABULOUSO when you’re preggers.
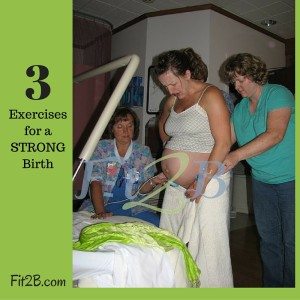
Beyond the exercises I teach in my videos, though, I think the best motions any pregnant woman should do are aligning, walking, and squatting. Sometimes, our pregnant bodies object to these basic things, so here are more resources.
Resources:
- Preview our Fit2B Mom section which mirrors our Prenatal Fitness Program, minus the email support, weekly reminders, and lifetime access.
- Read my article on the 3 best exercises for pregnancy and birth.
- Visit TurningBaby.com for moves YOU can do to assure your baby’s correct alignment for birth.
- If you stink at squats, this free squatting tutorial video shows you how to make safe progress.
6. Do you have any tips for pushing and positioning during labor?
Most clinical physiotherapists I collaborate with report that it’s often the pushing phase that widens a diastasis recti the most, and I agree!
My colleagues and I have all had our hands in the gaps of clients’ bellies who had little to no separation throughout most of their pregnancies. Then they have a traumatic birth, or a hard pushing phase, or a Cesarean or episiotomy during which muscles get sliced apart, causing major nerve damage. Often, the next time we see them, their DRA is wider than it was during pregnancy!
I am doing everything I possibly can within my scope here on this fitness platform to empower women with education and strategic exercises that will help them connect to their core in ways that will improve their pushing techniques and reduce their risk of birth-related injury. I have something for everyone, professionals and pregnant (or both) and whenever I learn something new, I pass it on.
 Resources
Resources
- The motions in my “Labor Prep” routine—included in the Fit2B Prenatal Fitness Program.
- Experts In Diastasis Recti e-course for members of the public and professionals alike. (Professionals: 6 CEC/CEUs)
- I love the tips in the last half of this “Natural Mama” article by Katy Bowman.
- Online prenatal core “prehab” with The Tummy Team.
- “The Importance of Core Strength in the Prenatal & Postnatal Client.” (7 CEC/CEUs)
7. How can I protect my pelvic floor during pregnancy and delivery?
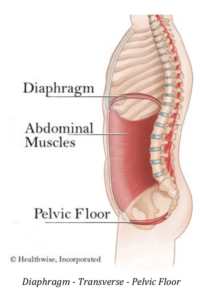 Your pelvic floor is the base of your core cylinder. Your pelvic floor muscle group (PFMG) is affected by pregnancy as well as labor and delivery, and a surgical birth doesn’t negate that. In the 2018 Birth Healing Summit, several expert speakers emphasized that a Cesarean section may actually worsen certain pelvic floor and core symptoms.
Your pelvic floor is the base of your core cylinder. Your pelvic floor muscle group (PFMG) is affected by pregnancy as well as labor and delivery, and a surgical birth doesn’t negate that. In the 2018 Birth Healing Summit, several expert speakers emphasized that a Cesarean section may actually worsen certain pelvic floor and core symptoms.
So again, I cannot pass up another chance to sing the praises of pelvic floor PT when it comes to addressing anything concerning your cootchie. Hands-on clinical evaluation and treatment will help resolve your personal pain and dysfunction, and I work hard to be sure that Fit2B exercise routines won’t undo that rehab.
(A note on my word selection: this website is for all women around the world who all have different names for their vulva, vagina, and pelvic floor area, so they use various search terms to find us. My mom thought the word “butt” was distasteful, so our family said “fanny”—which I have used in a couple videos and shocked a few of our clients. However, since there are no “bad” body parts, I refuse to acknowledge any body-part word as bad. I hereby reclaim all the words for all the fearfully and wonderfully made parts!)
Back To Resources For Pelvic Floors:
- Your local women’s health pelvic physical therapist. 😉
- Read my article about “Leaking Urine During {or After} Exercise.”
- Read this abstract of a study showing how the transverse abs co-activate with your pelvic floor.
- Take our Foundational Five Plus ecourse for access to exercise videos and support that help you safely reconnect to your abs and pelvic floor as you resume your workouts.
- Read yet another abstract mentioning how 66% of women with DRA have at least one support-related pelvic floor dysfunction, such as incontinence or prolapse (Spitznagle et al 2007).
“For those of you dealing with prolapse/leaking issues I just wanted to share my story. I have had 7 babies and had a cervical prolapse after #5 was born. When I first started running before I as working on my core I could barely make it 10-15 minutes without stopping to use the bathroom, even if I had just used it before starting to exercise. Today I ran for over an hour and had absolutely no issues. I can do jumping jacks, too! I remember being in that place where I thought I was doomed to a life of having to wear a pad when I exercised, but after healing my diastasis and focusing on alignment and strengthening my pelvic floor it got better. I started Fit2B in May 2012 and I would say the problem was nearly resolved after about 5-6 months. It’s not a quick fix, but I truly believe that as long as I keep core strength as a priority it will be a permanent fix 🙂 “ –Alison P.
8. Do you have any tips for C-section scars?
Honestly, this isn’t something I get asked by pregnant women who are planning surgical births, but I wish they would. It’s quite important for you to know that scar tissue likes to spread. Women’s health physical therapists are tracing pelvic pain and even shoulder issues to the impact of scar tissue from years-old Cesarean wounds.
Like Diane Lee commented during the 2018 Birth Healing Summit, if someone stabs you in the stomach, it’s called assault and you get all kinds of therapy. If you have a C-section, it’s called minor surgery and you’re sent home with a baby. You’re given all kinds of instructions for the baby, but not for your own self-care.
So let me offer two pieces of advice: take excellent care of your healing wound, and watch the scar massage video below. Scar massage can help break up fascial adhesions so that the muscles begin to “slide” back and forth again like they’re supposed to, plus it also helps reduce numb sensations.
9. How soon after I give birth should I start exercising?
If you define exercise as strenuous, weight-lifting or cardio-style movements that elevate your heart rate for longer than 15-20 minutes at a time, then PLEASE WAIT until you’re cleared by your doctor and/or physical therapist to resume that sort of exercising. (Then again, chasing a toddler also fits that definition, haha!)
Now seriously, I’m a big fan of letting all your big muscles TAKE IT SLOW for 6-12 weeks after you give birth. You just made a baby, delivered a baby, and now you’re feeding and caring for that baby (all on very little sleep), so it’s NOT the time to go back to long, heart-pumping workouts.
 It’s time to rest and schedule yourself for pelvic PT and do your gentle belly breaths + all the gentle, seated work such as shoulder & neck stretches that don’t feel like they count on a normal day but which feel so yummy.
It’s time to rest and schedule yourself for pelvic PT and do your gentle belly breaths + all the gentle, seated work such as shoulder & neck stretches that don’t feel like they count on a normal day but which feel so yummy.
You can and should begin utilizing the core breath as you move your body and lift your baby immediately after birth.
I teach the core breath (belly breath) in our most basic exercise routines which have been approved and recommended by midwives and physicalt therapists for use just 3 days after vaginal birth or 10 days after surgical birth, at which point you should also consider:
• Taking a short, slow walk. Walking is the best. It will flex and stretch your core and pelvic floor in a natural way. So, take a stroll around your neighborhood while smelling your newborn’s head and showing off to the neighbors.
• Use a baby-wearing wrap that supports your belly firmly but gently like a hug. Read this article I wrote for my top 5 dos and don’ts of babywearing.
• Set up your appointment with a local pelvic floor physiotherapist or diastasis rehab specialist. You’ll be so grateful you did, because you’ll get your body back without hurting yourself and without loads of hard work.
• Utilize Fit2B Studio’s pathway of workouts just for pregnant and post-partum moms. The routines in Fit2B’s New Mom section are gentle, gentle, gentle, and full of oh-so-healing and feel-good moves.
10. What do I really need to know about exercising post-Cesarean section?
 The following is a direct quote from my colleague Lorraine Scapens who contributed to the topic of C-sections and diastasis for our Experts on Diastasis Recti eCourse which you can purchase here.
The following is a direct quote from my colleague Lorraine Scapens who contributed to the topic of C-sections and diastasis for our Experts on Diastasis Recti eCourse which you can purchase here.
Lorraine stated the following:
“For moms who have had a C-section (be that elective or emergency), rest is the most powerful form of recovery. This does not mean moms who have had a C-section shouldn’t or can’t exercise—because they can. Specific rehabilitation exercises will improve recovery, make daily tasks easy, and improve mom’s emotional well-being.
I would suggest that, directly following a C–section, Mums use a specific C–section binder (I promote ABDOMEND) and ensure good nutrition. From 2 weeks onwards, I suggest a daily program of TA [transverse abdominus] and PFM [pelvic floor muscle] activation exercises when the mom is lying on the floor, standing, sitting, breastfeeding, and holding baby. Once a 2-week activation program is followed, rehabilitation exercises can be added. Moms generally start following our Birth2FitMum program from 4-5 weeks post C–section.”
And I would add that Lorraine’s programming complements mine quite well if you’re looking for some variety from the other side of the world! Love her!
11. I’ve had a Cesarean section, but I want to have a vaginal birth (VBAC) next time. How can I prepare my pelvic floor for that?
The answer to this comes from my Canadian colleague,  Kim Vopni, also known as The Fitness Doula.
Kim Vopni, also known as The Fitness Doula.
Here’s Kim’s answer to this question:
“When you are planning a VBAC, the preparation for your pelvic floor is essentially the same as you would do if this was your first or subsequent vaginal birth.”
Here are some free tips:
- Optimize your pelvic floor by paying attention to your alignment, posture, breathing, etc.
- See a pelvic floor physio—they will not typically do internal work when you are pregnant unless there is something key to work on, but they can help align and balance the pelvis and guide you with posture and breathing. They’ll also help mobilize the scar tissue from your cesarean birth to ensure your core is working well for your pregnancy and your birth.
- Ensure you are doing functional pelvic floor exercise—first learn to contract and release your pelvic floor, and then choose movements that incorporate the pelvic floor like squats, lunges, and bridges.
- Perineal massage in the last 3-5 weeks.
- Learn different birth positions so you can practice them ahead of time.
Kim also went on to say the following:
“Cesarean births are major abdominal surgery and can leave a woman’s core a bit out of sorts. The muscles and tissues in the abdominal wall have been displaced, cut, and stretched. The nerves have been stretched and compressed as well, and this often results in a lack of sensation or feeling in the abdomen and pelvic floor. The nerves are responsible for communicating with the muscles, and when they have been injured it can affect the ability of the muscles to work properly.
“Also, the adhesions that are left behind after the surgery can affect the muscles, as well, if they happen to be pulling them out of alignment or ‘sticking’ to somewhere they shouldn’t be. The best bet is to work with a pelvic floor physiotherapist who can help release the scar tissue and adhesions as well as help you connect with your pelvic floor again. Biofeedback can often be helpful as it will allow you to ‘see’ even if you can’t ‘feel.’
“In an ideal world, pelvic floor activation and breath work, done ASAP after the surgery, is ideal to help regenerate the nerves and lessen the long-term challenges. In an ideal world, women have learned how to activate their pelvic floor properly before pregnancy and birth, so that even if they lose some sensation they still know how to activate it and have a better chance of regenerating the muscles and nerves.”
Resources:
- Kim’s Prepare To Push program is excellent.
- Kim is also the contributing pelvic floor pro in our Experts on Diastasis Recti eCourse.
- If you’re already a member of Fit2B, you should do this Pelvic Floor Connections routine.
We welcome further questions. Please fill out a contact form.
*Please Note: This page contains affiliate links that earn the founders of Fit2B Studio a commission if you choose to purchase them. Not every item linked earns us a commission. This is one more way you can support the families running this business. Thank you!
5 thoughts on “Pregnancy Q & A”
Comments are closed.



Pingback: Our Favorite Things: Pregnancy & Postpartum – The Sojourning Dunns
Pingback: How to Identify and Fix Diastasis Recti | Wellness Mama
Pingback: Breastfeeding Weight Loss: How to Get Your Body Back AFTER BABY?
Pingback: Fit2B™ New Mamas | Fit2B Studio
Pingback: All the Little Things About Squats